The Studies
Diseases of the heart and blood vessels are the number one cause of death in the U.S. Researchers in this Research Focus Area at NEOMED integrate research in physiology, pharmacology, molecular and cellular biology, and bioinformatics. Ultimately, the goal is to improve health outcomes for patients by contributing knowledge about the hearth and blood vessels and their diseases.
A partner’s perspective
Joseph Pietrolungo, D.O., of Summa Health System discusses the importance of heart and blood vessel disease research for developing novel treatments.
VIDEO EXTRA: Diseases of the heart and blood vessels are the number one cause of death in the U.S. Researchers in the Heart and Blood Vessel Disease Research Focus Area at NEOMED advance the understanding of these diseases with the goal of going beyond stopping their progression and, ultimately, curing them.
The Statistics
$1.1 trillion
Overall impact of cardiovascular disease.
#1
Diseases of the heart & blood vessels are the number one cause of death in the U.S. accounting for more than $1/2 Trillion in healthcare costs.
30
Every thirty seconds an individual in the U.S. dies from sudden cardiac disease.
The Successes
- Creation of molecularly engineered stem cells to build bypasses in the heart.
- Discovery of the role that mechanical factors play in tumor blood vessel growth.
- Discovery of the critical role of bioenergetics in cell growth.
- Discovery that heart failure may be a disease of both blood vessels and cardiac muscle.
- Discovery that a cell type in the heart that makes it stiff, may be mechanically activated.
- Implementation and completion of a Phase 1 clinical trial in which a drug is given to patients to recruit stem cells to the heart to treat heart failure.
- Discovery of a bone marrow stem that plays a role in blood vessel growth in the heart.
- Discovery that the growth blockages in blood vessels is modulated by certain hormones released by fat. These hormones make an injured blood vessel more prone to injury.
The Scientists
Research within the Heart and Blood Vessel Disease Research Focus Area is comprised of four clusters of investigators in different scientific ares with a focus on heart and blood vessel diseases.
Ischemic Heart Disease & Heart Failure
Stem Cell & Regenerative Medicine
The Stories
- Read more
“Although Aesculapius himself applies the herbs, by no means can he cure a wound of the heart.” To be sure, progress has been made since the Roman poet Ovid wrote […]
- Read more
How can you mend a broken heart? Flowers? Chocolate? Perhaps, simply saying, “I’m sorry!?” Of course, there are times where it might cost you a little more — think diamonds, […]
CONTACT
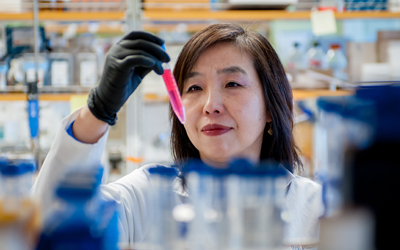
Liya Yin, M.D., Ph.D., FAHA, FCVS
Director, Heart & Blood Vessel Disease Research Area
Phone: 330.325.6521
Email: lyin@neomed.edu